Cognitive Challenges from Cancer and Its Treatments
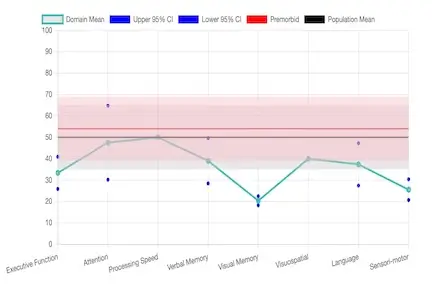
Cancer treatments—including chemotherapy, endocrine therapy, targeted therapy, and immunotherapy—can lead to cancer-related cognitive impairment (CRCI). Symptoms include memory lapses, trouble concentrating, slower thinking, and difficulties with planning or problem-solving. CRCI may persist for months or years after treatment due to factors such as neurotoxicity, inflammation, hormonal changes, fatigue, and depression.
The American Cancer Society and American Society of Clinical Oncology recommend screening for cognitive symptoms and referring patients to neuropsychologists for evaluation and cognitive rehabilitation.[1-8]
Helpful resource: This Is Your Brain On Chemo
Cognitive Challenges from Chronic Illnesses
Cognitive challenges associated with chronic illnesses such as diabetes, multiple sclerosis (MS), Parkinson’s disease, chronic kidney disease, heart disease, stroke, lupus and other autoimmune conditions, chronic fatigue syndrome, and fibromyalgia include deficits in attention, processing speed, executive function, and memory. These impairments are multifactorial, involving direct disease effects on the central nervous system, neuroinflammation, vascular injury, metabolic dysregulation, and comorbid symptoms such as fatigue, pain, and depression.
Specific Conditions
- Diabetes: Slowed mental and motor processing, reduced attention, and impaired executive function. Type 2 diabetes often affects learning and memory, with chronic hyperglycemia, insulin resistance, and microvascular disease contributing to deficits.[9-13]
- Multiple Sclerosis (MS): Commonly impairs processing speed, memory, and executive function, correlating with lesion burden and neuroinflammation.[14]
- Parkinson’s Disease: Executive function, attention, and visuospatial abilities are affected, sometimes progressing to dementia due to dopaminergic and other neurotransmitter dysfunction.
- Chronic Kidney Disease & Heart Disease: Global cognitive slowing, attention deficits, and impaired memory due to vascular injury and metabolic disturbances.[16]
- Stroke: Focal deficits depending on lesion location, often affecting attention, executive function, and memory.
- Lupus & Autoimmune Conditions: Executive dysfunction and attention deficits due to CNS involvement or neuroinflammation, exacerbated by fatigue and depression.[14-15]
- Chronic Fatigue Syndrome & Fibromyalgia: Impairments in working memory, attention, and executive function (“fibrofog”), worsened by pain, sleep disturbances, and mood disorders.[17]
How Neuropsychology Can Help
Neuropsychologists play a vital role in supporting patients with cognitive changes from cancer, chronic illnesses, or brain injury. Their goal is to help individuals regain mental clarity, improve daily functioning, and enhance overall quality of life. Here’s how they do it:
- Comprehensive Cognitive Assessment: Neuropsychologists perform detailed evaluations to identify specific strengths and weaknesses in memory, attention, processing speed, and executive function. These assessments help pinpoint which areas are most affected and guide targeted interventions.
- Addressing Modifiable Factors: Many cognitive challenges are influenced by treatable factors such as depression, anxiety, fatigue, sleep disturbances, pain, or medication side effects. Neuropsychologists collaborate with patients and healthcare teams to manage these contributors, reducing their impact on thinking and daily functioning.
- Emotional and Psychological Support: Adjusting to cognitive changes can be stressful. Neuropsychologists provide counseling and psychoeducation to help patients and families understand their symptoms, build coping strategies, and maintain motivation throughout recovery.
- Integration with Multidisciplinary Care: Neuropsychology does not work in isolation. By coordinating with oncologists, neurologists, primary care providers, occupational therapists, and speech-language pathologists, neuropsychologists ensure that cognitive care is seamlessly integrated into the overall treatment plan.
- Cognitive Rehabilitation: Tailored programs may include memory exercises, attention training, problem-solving practice, compensatory strategies, and behavioral modifications. These interventions help patients develop practical skills to cope with cognitive difficulties, improve work or school performance, and enhance adherence to medical treatment plans.[1][4-5][8]
Helpful resource: The Brainpower Boosting Activity Workbook for Adults
References
- American Cancer Society/American Society of Clinical Oncology Breast Cancer Survivorship Care Guideline. Runowicz CD, Leach CR, Henry NL, et al. Journal of Clinical Oncology. 2016;34(6):611-35. doi:10.1200/JCO.2015.64.3809.
- Lange M, Joly F, Vardy J, et al. Cancer-Related Cognitive Impairment: An Update on State of the Art, Detection, and Management Strategies in Cancer Survivors. Ann Oncol. 2019;30(12):1925-1940. doi:10.1093/annonc/mdz410.
- Fleming B, Edison P, Kenny L. Cognitive Impairment After Cancer Treatment: Mechanisms, Clinical Characterization, and Management. BMJ. 2023;380:e071726. doi:10.1136/bmj-2022-071726.
- Sheppard DP, Noll KR, Wefel JS, Bradshaw ME. Neuropsychological Evaluation for Oncology. Neurol Clin. 2024;42(4):875-887. doi:10.1016/j.ncl.2024.05.012.
- Vannorsdall TD. Cognitive Changes Related to Cancer Therapy. Med Clin North Am. 2017;101(6):1115-1134. doi:10.1016/j.mcna.2017.06.006.
- Joly F, Giffard B, Rigal O, et al. Impact of Cancer and Its Treatments on Cognitive Function: Advances in Research From the Paris International Cognition and Cancer Task Force Symposium and Update Since 2012. J Pain Symptom Manage. 2015;50(6):830-841. doi:10.1016/j.jpainsymman.2015.06.019.
- Lomeli N, Lepe J, Gupta K, Bota DA. Cognitive Complications of Cancer and Cancer-Related Treatments - Novel Paradigms. Neurosci Lett. 2021;749:135720. doi:10.1016/j.neulet.2021.135720.
- Noll KR, Bradshaw ME, Rexer J, Wefel JS. Neuropsychological Practice in the Oncology Setting. Arch Clin Neuropsychol. 2018;33(3):344-353. doi:10.1093/arclin/acx131.
- Pignalosa FC, Desiderio A, Mirra P, et al. Diabetes and Cognitive Impairment: A Role for Glucotoxicity and Dopaminergic Dysfunction. Int J Mol Sci. 2021;22(22):12366. doi:10.3390/ijms222212366.
- McCrimmon RJ, Ryan CM, Frier BM. Diabetes and Cognitive Dysfunction. Lancet. 2012;379(9833):2291-9. doi:10.1016/S0140-6736(12)60360-2.
- Zhang S, Zhang Y, Wen Z, et al. Cognitive Dysfunction in Diabetes: Abnormal Glucose Metabolic Regulation in the Brain. Front Endocrinol. 2023;14:1192602. doi:10.3389/fendo.2023.1192602.
- Ryan CM, van Duinkerken E, Rosano C. Neurocognitive Consequences of Diabetes. Am Psychol. 2016;71(7):563-576. doi:10.1037/a0040455.
- Zilliox LA, Chadrasekaran K, Kwan JY, Russell JW. Diabetes and Cognitive Impairment. Curr Diabetes Rep. 2016;16(9):87. doi:10.1007/s11892-016-0775-x.
- Restrepo-Martinez M, Bell V, Ramirez-Bermudez J. Cognitive Disorders in Patients With Neuroimmunological Disease. Curr Opin Psychiatry. 2025;38(2):126-133. doi:10.1097/YCO.0000000000000977.
- Shaw BC, Anders VR, Tinkey RA, et al. Immunity Impacts Cognitive Deficits Across Neurological Disorders. J Neurochem. 2024;168(10):3512-3535. doi:10.1111/jnc.15999.
- Gasquoine PG. Cognitive Impairment in Common, Noncentral Nervous System Medical Conditions of Adults and the Elderly. J Clin Exp Neuropsychol. 2011;33(4):486-96.
- Glass JM. Fibromyalgia and Cognition. J Clin Psychiatry. 2008;69 Suppl 2:20-4.