What Are CPT Codes and the Neuropsychology Superbill?
CPT codes (Current Procedural Terminology) are the standard billing identifiers used by healthcare providers, including neuropsychologists, to describe services rendered. Since we operate on a Direct Access (self-pay) model, we provide a Superbill—a detailed, itemized receipt that includes the CPT codes and ICD-10 diagnostic codes. This allows patients to submit a claim for out-of-network reimbursement from their commercial insurance company, helping recover a portion of their investment.
Essential Neuropsychology CPT Codes and Billing Units
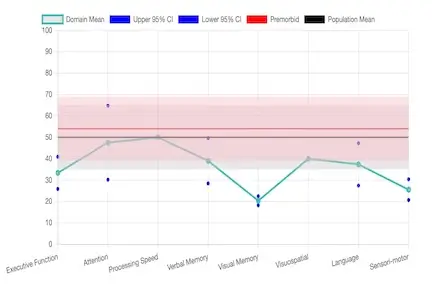
Understanding these time-based codes is crucial for predicting potential reimbursement. The total number of units billed reflects the comprehensive work involved in a full evaluation, including direct patient time and indirect time (scoring, interpretation, report writing).
- 90791: Initial Psychiatric Diagnostic Interview. The first step covering comprehensive history and diagnostic interviewing. Typically the most reliably covered service, even via telehealth (-95 modifier) in Florida.
- 96116: Neurobehavioral Status Exam. A brief assessment of cognitive and behavioral functioning, often used for follow-up or screening. Coverage varies by insurer.
- 96132 (First Hour) / 96133 (Each Additional Hour): Neuropsychological Testing Evaluation Services. Billed by the neuropsychologist for professional time spent on test selection, data integration, interpretation, clinical decision-making, and report writing.
- 96136 (First 30 Min) / 96137 (Each Additional 30 Min): Neuropsychological Test Administration & Scoring. Time spent by the qualified health care professional personally administering and scoring standardized tests. A full battery often requires 12–20+ units.
Insurance Coverage: Medical Necessity and Out-of-Pocket Costs
Insurance coverage for neuropsychology hinges entirely on medical necessity. This determines which CPT codes are covered and which specific conditions qualify for reimbursement.
What Insurance Often Covers (Even Out-of-Network)
- Initial diagnostic interviews like 90791 are the most reliably covered service as they establish the need for further testing.
- Telehealth for interviews (90791-95, 96116-95) is commonly reimbursed by most commercial plans.
- Evaluations following acute neurological events such as stroke, TBI, or confirmed neurodegenerative disorders like Alzheimer’s disease.
Diagnoses Typically NOT Covered (Lack of Medical Necessity)
Insurance companies only reimburse when the evaluation is deemed medically necessary (e.g., post-TBI, stroke, or moderate cognitive decline). The following are routinely denied, meaning they are primarily out-of-pocket expenses:
- ADHD Testing: Assessment primarily for inattention or executive dysfunction in adults without a neurological or severe psychiatric comorbidity is often denied coverage.
- Learning Disabilities & Psychoeducational Testing: Evaluations for dyslexia, dyscalculia, or school performance issues are categorized as educational, not medical.
- Legal/Career/Baseline Testing: Testing conducted solely for workplace accommodations, forensic/legal purposes, or general baseline neurocognitive testing (if the PCP deems complaint subjective or an initial screener shows no deficit) is not covered.
- Family Risk Without Current Symptoms: Evaluations requested solely due to a family history of dementia or psychiatric illness without current cognitive symptoms is frequently denied.
The Reality of Full Testing Coverage (96132, 96136)
Full neuropsychological batteries (96132, 96133, 96136, 96137) are frequently considered out-of-pocket expenses or reimbursed at a very partial rate, whether remote or in-person. The exception is generally for clear, acute neurological injury (e.g., TBI, stroke).