Protecting Your Brain Through Heart Health: Neuropsychological Evaluation for Cognitive Decline Risk
Heart disease and cognitive decline affect people of all backgrounds, including celebrities. Notable examples include Rosie O'Donnell, Toni Braxton, Larry King, Kelsey Grammer, and Kevin Smith.
Heart health and cognitive health are closely linked, with strong evidence showing that cardiovascular risk factors and diseases significantly increase the risk of cognitive decline and dementia. Cardiovascular diseases—including heart failure, atrial fibrillation (AFib), and coronary heart disease—are associated with structural brain changes, covert brain infarction, and cognitive impairment. Mechanistically, these links are mediated by shared risk factors such as hypertension, diabetes, obesity, and smoking, as well as cerebral hypoperfusion, microvascular injury, inflammation, and neurodegeneration. For example, heart failure and subclinical cardiac dysfunction are associated with smaller total brain and hippocampal volumes, which are markers of neurodegeneration and predictors of cognitive decline. [1-3]
The Role of Modifiable Risk Factors in Preventing Vascular Cognitive Impairment
The American Heart Association’s Life’s Simple 7—nonsmoking, healthy diet, physical activity, optimal body weight, and control of blood pressure, cholesterol, and glucose—are protective not only against cardiovascular disease but also against cognitive decline. Higher cardiovascular health scores are associated with slower cognitive decline and reduced dementia incidence, even in older adults. [4-6] Coronary heart disease increases the risk of cognitive impairment and dementia by about 45%, while atrial fibrillation and heart failure independently raise the risk of cognitive decline due to cerebral hypoperfusion, embolic events, and microvascular injury. [1-3]
Emerging research highlights the utility of cardiac biomarkers such as natriuretic peptides and troponins to predict structural brain changes and cognitive impairment, underscoring the importance of early identification and management of cardiac dysfunction. [2,8] Optimizing cardiovascular health throughout life is a key strategy for maintaining cognitive health and reducing the risk of dementia, emphasizing the need for integrated prevention and management of cardiovascular and brain health. [1,4-6,9]
Neuropsychology Bridges Heart and Brain Health: Early Detection of Cognitive Impairment in Cardiac Patients
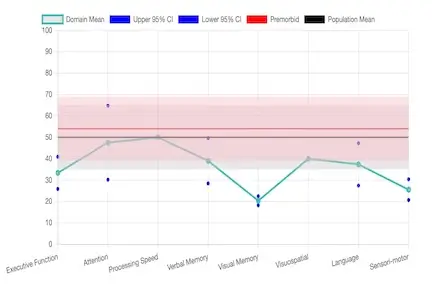
Neuropsychology plays a pivotal role in assessing cognitive health in patients with cardiovascular disease. Cognitive impairment is prevalent among individuals with cardiac conditions, yet up to half of cases may go unrecognized without formal neuropsychological evaluation. [1] Standardized neuropsychological testing detects subtle deficits across memory, executive function, attention, and processing speed—domains frequently affected by cardiac dysfunction. [2,3]
Routine neuropsychological assessment is essential because cognitive impairment can directly impact medication adherence, self-management, and the ability to participate in complex treatment regimens. [1] Neuropsychologists collaborate with cardiologists and other specialists to interpret cognitive profiles, differentiate vascular from neurodegenerative etiologies, and guide individualized care plans. Incorporating neuropsychological evaluation into cardiovascular care improves detection, management, and outcomes for patients with comorbid heart and cognitive disorders. [1,3]
Take Action: Schedule a Telehealth Cognitive Assessment for Atrial Fibrillation and Heart Risk in Florida
Heart and brain health are connected. Protecting your cardiovascular system is crucial to safeguarding cognition. Individuals with a history of heart disease, atrial fibrillation, coronary heart disease, or other cardiac risk factors should consider a neuropsychological evaluation to detect early cognitive changes and develop a personalized management plan.
Dr. Davis provides tele-neuropsychology and in-person assessments across Florida, covering ADHD, dementia, TBI, chronic illness cognitive decline, and pre-surgical evaluations. Our direct-access model bridges gaps in specialty care, offering fast scheduling and transparent pricing for patients seeking timely cognitive health evaluation.
References
- Testai FD, Gorelick PB, Chuang PY, et al. Cardiac Contributions to Brain Health: A Scientific Statement From the American Heart Association. Stroke. 2024;55(12):e425-e438. doi:10.1161/STR.0000000000000476
- Yaqub A, Bis JC, Frenzel S, et al. Clinical and Imaging Markers of Cardiac Function and Brain Health: A Meta-Analysis of Community-Based Studies. Neurology. 2025;104(8):e213421. doi:10.1212/WNL.0000000000213421
- Xu C, Tao X, Ma X, Zhao R, Cao Z. Cognitive Dysfunction After Heart Disease: A Manifestation of the Heart-Brain Axis. Oxidative Medicine and Cellular Longevity. 2021;2021:4899688. doi:10.1155/2021/4899688
- Samieri C, Perier MC, Gaye B, et al. Association of Cardiovascular Health Level in Older Age With Cognitive Decline and Incident Dementia. JAMA. 2018;320(7):657-664. doi:10.1001/jama.2018.11499
- Gorelick PB, Furie KL, Iadecola C, et al. Defining Optimal Brain Health in Adults: A Presidential Advisory From the American Heart Association/American Stroke Association. Stroke. 2017;48(10):e284-e303. doi:10.1161/STR.0000000000000148
- Pase MP, Beiser A, Enserro D, et al. Association of Ideal Cardiovascular Health With Vascular Brain Injury and Incident Dementia. Stroke. 2016;47(5):1201-1206. doi:10.1161/STROKEAHA.115.012608
- Deckers K, Schievink SHJ, Rodriquez MMF, et al. Coronary Heart Disease and Risk for Cognitive Impairment or Dementia: Systematic Review and Meta-Analysis. PLoS One. 2017;12(9):e0184244. doi:10.1371/journal.pone.0184244
- Jensen M, Zeller T, Twerenbold R, Thomalla G. Circulating Cardiac Biomarkers, Structural Brain Changes, and Dementia: Emerging Insights and Perspectives. Alzheimer's & Dementia. 2023;19(4):1529-1548. doi:10.1002/alz.12926
- Lazar RM, Howard VJ, Kernan WN, et al. A Primary Care Agenda for Brain Health: A Scientific Statement From the American Heart Association. Stroke. 2021;52(6):e295-e308. doi:10.1161/STR.0000000000000367