Why Neuropsychological Testing Is the Gold Standard for Memory & Neurocognitive Concerns
Neuropsychological testing is the most precise and evidence-based method for evaluating memory loss, attention problems, executive dysfunction, and neurocognitive decline. Unlike brief screening tools or imaging alone, a comprehensive neuropsychological evaluation examines how the brain is functioning in real time using standardized, psychometrically validated measures. This is the quality of care we offer to individuals across the state.
For individuals and families in the region, obtaining an accurate neuropsychological testing Florida diagnosis is the first critical step toward effective treatment. Neuropsychologists are uniquely trained to answer critical questions—like differentiating normal aging from early dementia—using objective data rather than guesswork.
When to Consider Neuropsychological Testing for Memory Problems
Many patients seeking a neuropsychologist for memory problems near me describe symptoms such as:
- Forgetting recent conversations or appointments
- Difficulty finding words or following conversations
- Problems managing finances, medications, or planning
- Increased confusion under stress or fatigue
- Neurocognitive changes after concussion, illness, or surgery
A comprehensive evaluation helps differentiate normal forgetfulness from mild cognitive impairment (MCI), dementia, traumatic brain injury (TBI), or mood-related neurocognitive changes.
The Scientific & Psychometric Foundation of Neurocognitive Assessment: Going Deeper
Neuropsychology is grounded in psychometrics—the science of psychological measurement. Every test used in a valid neuropsychological evaluation has undergone rigorous statistical validation to ensure reliability, sensitivity, and clinical relevance. This is why psychometric neurocognitive testing is essential for a truly objective assessment.
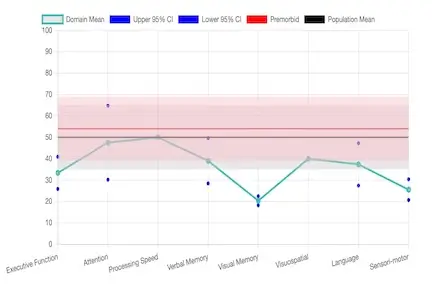
The Role of Normative Data and Standard Scores
The core of psychometrics in this field is the use of Normative Data. Each test score is not interpreted in a vacuum; it is compared to thousands of scores from a normative sample—a large, representative group of healthy individuals matched for age, education, gender, and sometimes ethnicity. This comparison process converts raw scores into Standard Scores (like T-scores or Z-scores), which tell us exactly how far an individual’s performance deviates from the average of their peers. For instance, a score that is two standard deviations below the mean is highly indicative of impairment. This rigorous standardization is what makes our services so powerful.
Key Psychometric Principles: Reliability and Validity
To ensure the data is trustworthy, tests must demonstrate two key psychometric properties:
- Reliability: The consistency of the measure. If the test is repeated, will it produce the same results (e.g., test-retest reliability)? Consistency allows us to confidently track neurocognitive change over time, crucial for mild cognitive impairment testing.
- Validity: The accuracy of the measure. Does the test truly measure what it claims to measure? Construct Validity ensures the test accurately reflects the neurocognitive domain (like 'working memory'), while Ecological Validity ensures the test results predict real-world functioning (like managing finances or driving ability).
Commonly used instruments for neuropsychological testing in Florida include:
- Wechsler Adult Intelligence Scale (WAIS): Assesses reasoning, working memory, processing speed, and verbal comprehension.
- Wechsler Memory Scale (WMS): Evaluates immediate and delayed verbal and visual memory.
- California Verbal Learning Test (CVLT): Measures learning efficiency, recall patterns, and recognition memory, often revealing subtle differences between neurodegenerative and mood-related memory issues.
- Trail Making & Executive Function Tests: Assess attention, mental flexibility, and processing speed, vital for TBI neurocognitive assessment Florida.
- NIH Toolbox Cognition Battery: Provides nationally normed assessment of multiple neurocognitive domains, supporting a comprehensive objective neurocognitive decline evaluation.
These tools allow clinicians to compare an individual’s performance to age- and education-matched norms, identifying even subtle changes that may not appear on routine medical exams.