Understanding Postoperative Cognitive Dysfunction (POCD) and Anesthesia
It's common for patients to worry about feeling lasting brain fog after anesthesia or noticeable memory loss after surgery. While some fuzziness is expected right after a procedure, persistent difficulties with memory, attention, and executive function are classified as Postoperative Cognitive Dysfunction (POCD).
Anesthesia and surgery can trigger a range of anesthesia cognitive effects, from immediate, acute confusion to persistent issues that last for weeks or even months. The overall impact depends heavily on factors like your age, any chronic medical conditions you may have, your cognitive function before the procedure (your baseline memory status), and the type of surgery performed [1].
POCD vs. Postoperative Delirium
These two terms sound similar, but they describe very different conditions:
- Postoperative Delirium (POD): This is a serious, acute state of severe confusion and inattention, usually starting immediately after surgery or within the first few days. Delirium involves drastic changes in awareness, often appearing as agitation or severe lethargy. This requires immediate medical attention [1].
- Postoperative Cognitive Dysfunction (POCD): This is a more subtle decline in thinking skills (memory, speed, attention) that lasts long after hospital discharge. Patients with POCD are lucid—they know where they are—but they are simply not thinking as sharply as they were before the operation.
Prevalence and Symptoms of POCD
POCD is a widespread concern. It is characterized by measurable declines in key thinking skills:
- Memory Loss: Trouble remembering new information or recalling recent events.
- Attention Problems: Difficulty concentrating, focusing on tasks, or managing complex information flow.
- Slowing Down: Reduced processing speed, making it hard to keep up with conversations or finish tasks efficiently.
- Executive Dysfunction: Problems with planning, organizing, multi-tasking, and making sound judgments.
For middle-aged adults undergoing major noncardiac surgery, POCD affects about 10–13% at three months. These rates can be much higher—between 16% and 39%—after complex procedures like cardiac surgery [2].
Who is Most at Risk for POCD?
While POCD can affect anyone, your risk increases if you fall into any of these categories:
- Advanced Age: Being elderly is the single strongest risk factor.
- Pre-Existing Cognitive Issues: If you already had Mild Cognitive Impairment (MCI) or early signs of memory change, your brain is more vulnerable.
- Type and Length of Surgery: Longer, more invasive surgeries, especially those involving the heart or major joints, carry a higher risk [7].
- Poor Health Before Surgery: Uncontrolled conditions like high blood pressure, diabetes, and other chronic medical conditions that affect blood flow to the brain.
- Genetic Factors: Some individuals, particularly those carrying the APOE ε4 allele (a risk factor for Alzheimer’s), may be more susceptible to long-term cognitive changes after surgery.
The Biology: Mechanisms of Anesthesia's Effects
The mechanisms of POCD and other anesthesia cognitive effects involve a biological 'one-two punch' to the brain. The stress of surgery combined with anesthetic agents triggers complex reactions [3]:
- Neuroinflammation: Both the surgery and the anesthetic can cause a temporary inflammatory response in the brain, which activates support cells called microglia. This 'brain inflammation' can impair communication between neurons [3].
- Memory Circuit Disruption: Anesthetics enhance the inhibitory chemical GABA in the brain. Sustained changes in this signaling can 'put the brakes' on the hippocampus, the critical region for forming new memories [4].
- Rhythm Changes: Anesthesia can disrupt the brain’s normal electrical rhythms (neural oscillations) needed for memory consolidation and focused attention [5].
Research confirms that managing inflammation and supporting the brain's natural signaling systems are key to recovery and preventing long-term cognitive changes after surgery [6].
Identifying Cognitive Changes with Neuropsychology
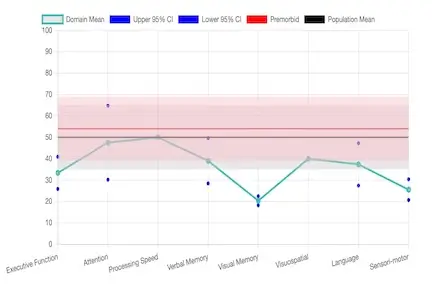
When brain fog after anesthesia lasts beyond the initial recovery period, a specialized assessment is needed. A neuropsychological evaluation Florida is the definitive way to objectively measure and understand these changes. Our services, including pre- and post-surgical cognitive assessment, are crucial because they:
- Establish Baseline: We conduct a pre-surgical assessment to know exactly how your brain functioned before the procedure, allowing us to measure change accurately.
- Pinpoint Deficits: We use validated tests (more detailed than basic screenings) to objectively measure declines in specific areas like memory and attention testing, processing speed, and executive function.
- Rule Out Other Causes: The evaluation determines if the problems are due to the surgery (POCD) or if other factors, such as depression, chronic pain, or medication side effects, are involved.
- Create a Roadmap: The findings guide a targeted treatment plan for cognitive recovery.
How Neuropsychology Supports Recovery
As neuropsychologists, we play a vital role in recovery by providing specialized cognitive rehabilitation after surgery and addressing all factors that might slow down healing:
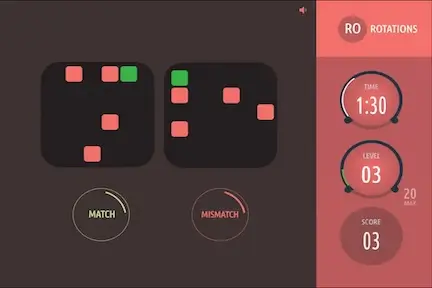
- Targeted Rehabilitation: We design customized programs including computer-based attention training and memory exercises tailored to your specific deficits found in the evaluation.
- Addressing Hidden Factors: We coordinate care to manage fatigue, sleep disturbances (like sleep apnea), anxiety, and chronic pain, as these severely compound cognitive symptoms.
- Teaching Compensation: We provide practical, real-world strategies—like utilizing digital calendars, simplifying routines, and optimizing the home/work environment—to help you manage daily life efficiently while your brain heals.
- Support and Guidance: We provide counseling and clear education for you and your family to reduce anxiety and manage expectations during the recovery process.
Prevention and Monitoring for Cognitive Health
The best approach to POCD is proactive management:
- Get Screened: If you are over 65 or have known memory issues, talk to your doctor about getting a comprehensive cognitive assessment or a short virtual screening before your surgery to establish a clear baseline.
- Optimize Health: Work with your primary care provider to aggressively manage risk factors like high blood pressure, diabetes, and cholesterol before the procedure.
- Stay Active: Engage in post-surgical cognitive stimulation, light physical activity (as cleared by your surgeon), and structured rehabilitation as soon as possible.
- Follow-up: Regular follow-up with a neuropsychologist or neurologist allows for tracking recovery progress and ensures the fastest possible return to your pre-surgical cognitive level.
References
- Evered LA, Silbert BS. Postoperative Cognitive Dysfunction and Noncardiac Surgery. Anesthesia and Analgesia. 2018;127(2):496-505. doi:10.1213/ANE.0000000000003514.
- Yang L, Chen W, Yang D, et al. Postsurgery Subjective Cognitive and Short-Term Memory Impairment Among Middle-Aged Chinese Patients. JAMA Netw Open. 2023;6(10):e2336985. doi:10.1001/jamanetworkopen.2023.36985.
- Zhang M, Yin Y. Dual Roles of Anesthetics in Postoperative Cognitive Dysfunction: Regulation of Microglial Activation. Front Immunol. 2023;14:1102312. doi:10.3389/fimmu.2023.1102312.
- Zurek AA, Yu J, Wang DS, et al. Sustained Increase in A5GABAA Receptor Function Impairs Memory After Anesthesia. J Clin Invest. 2014;124(12):5437-41. doi:10.1172/JCI76669.
- Liu H, Yang Z, Chen Y, et al. Neural Oscillations and Memory: Mechanisms of Anesthesia-Induced Amnesia. Front Neurosci. 2024;18:1492103. doi:10.3389/fnins.2024.1492103.
- Rump K, Adamzik M. Epigenetic Mechanisms of Postoperative Cognitive Impairment Induced by Anesthesia and Neuroinflammation. Cells. 2022;11(19):2954. doi:10.3390/cells11192954.
- Viderman D, Nabidollayeva F, Aubakirova M, et al. Postoperative Delirium and Cognitive Dysfunction After General and Regional Anesthesia: A Systematic Review and Meta-Analysis. J Clin Med. 2023;12(10):3549. doi:10.3390/jcm12103549.
- Mason SE, Noel-Storr A, Ritchie CW. The Impact of General and Regional Anesthesia on the Incidence of Post-Operative Cognitive Dysfunction and Post-Operative Delirium: A Systematic Review With Meta-Analysis. J Alzheimers Dis. 2010;22 Suppl 3:67-79. doi:10.3233/JAD-2010-101086.
- Reighard C, Junaid S, Jackson WM, et al. Anesthetic Exposure During Childhood and Neurodevelopmental Outcomes: A Systematic Review and Meta-analysis. JAMA Netw Open. 2022;5(6):e2217427. doi:10.0000000000000000.