Why Distinguishing Normal Aging from Dementia Matters
Many adults and families ask the same frightening question: “Is this just normal aging, or could it be dementia?” Occasional forgetfulness—such as misplacing keys or forgetting a familiar name—can be a common and non-threatening part of the normal aging process. However, persistent or worsening problems with memory and thinking may signal something more serious.
The key distinction between normal aging and dementia lies in functional impact rather than the mere presence of cognitive change. Normal aging involves mild, gradual changes that do not interfere with daily functioning, while dementia is defined by cognitive decline severe enough to impair independence in everyday activities.[1–2]
What Is Considered Normal Cognitive Aging?
As the brain ages, some cognitive changes are expected and considered benign. Normal cognitive aging may include:
- Decreased processing speed and reduced spontaneous recall
- Slower word retrieval ("tip-of-the-tongue" moments)
- Small declines in executive functioning[1]
Beginning in midlife, the ability to learn new information and recall it after a delay declines by approximately 10% per decade.[1] Nonverbal memory is often more affected than verbal memory, and recall is more affected than recognition. Importantly, normally aging adults can still learn new information—though more slowly—and retain well-learned knowledge nearly as effectively as younger adults.[1] Vocabulary, semantic knowledge, and procedural memory typically remain intact.[3]
Early Signs of Dementia That Warrant Evaluation
Dementia involves progressive cognitive decline that exceeds expectations for normal aging. Diagnostic criteria require impairment in at least two cognitive domains (or severe impairment in one domain per DSM-5) that represents decline from prior functioning and significantly interferes with daily life.[2]
- Repeatedly forgetting recently learned information
- Difficulty managing finances, medications, or schedules
- Problems completing previously routine tasks or impaired judgment[2]
When questions arise about forgetfulness vs dementia, relying on guesswork can delay appropriate medical, lifestyle, and planning interventions.[4]
How Neuropsychological Testing Differentiates Aging from Dementia
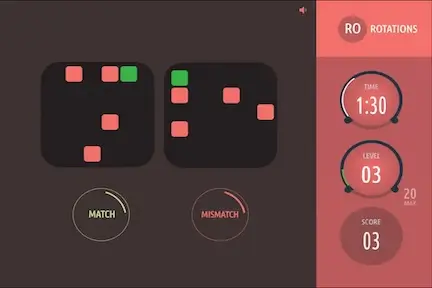
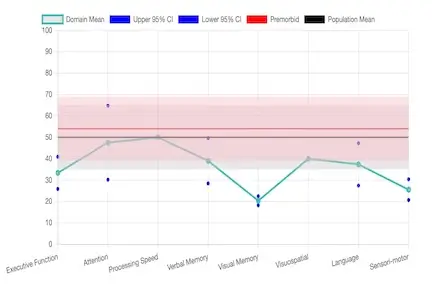
Neuropsychological testing in Florida uses standardized, psychometrically validated measures to assess memory, attention, language, executive functioning, and processing speed. Unlike brief cognitive screens, comprehensive testing produces a detailed cognitive profile.
Through an objective cognitive decline evaluation, neuropsychologists can determine whether symptoassessmentsms reflect:
- Normal aging
- Mild Cognitive Impairment (MCI)
- Alzheimer’s disease or other dementias (vascular, Lewy body, frontotemporal)
- Secondary effects of medical illness, medication interactions, mood, or stress
The Critical Role of Differential Diagnosis
One of the most valuable functions of neuropsychological testing is the differential diagnosis—the ability to rule out common, often reversible, causes of cognitive complaints. For instance, depression or chronic anxiety can mimic early dementia (sometimes called pseudodementia), causing severe complaints of memory and concentration loss. Testing patterns associated with mood disorders are distinctly different from those seen in neurodegenerative diseases like Alzheimer's. Similarly, cognitive slowing due to chronic pain, untreated sleep apnea, or medication side effects can be identified and separated from true neurodegenerative decline. This process ensures the patient receives the correct diagnosis and the most effective targeted treatment, whether that involves neurology, psychiatry, or lifestyle changes.
This diagnostic precision is critical because prognosis, treatment, and planning differ dramatically. Learn more about the science behind this process in our article on neuropsychology and psychometric testing.
The Neurobiological Distinction
Dementia is not simply accelerated aging—it represents a distinct pathological process. Normal aging involves reduced serine racemase expression and NMDA receptor down-regulation, whereas Alzheimer disease shows increased D-serine activity, NMDA receptor overstimulation, and neurotoxic cascades.[5–7]
Patterns of brain atrophy, neural network involvement, and rates of progression clearly differ between aging and neurodegenerative disease, underscoring the need for accurate diagnostic separation.[6]
The following framework illustrates how clinical presentation and underlying pathophysiology should be systematically separated when characterizing cognitive disorders:
Memory Loss in Adults Over 50: When to Seek Evaluation
A neuropsychological evaluation is recommended when:
- Symptoms worsen or accumulate over six months
- Daily functioning at work or home is affected
- There is a family history of early-onset dementia
- Neuroimaging is normal but cognitive symptoms persist
- Objective documentation is needed for work, disability, or care planning
Many individuals search for a neuropsychologist for memory problems near me after routine medical visits fail to provide clarity. Neuropsychological testing fills this diagnostic gap.